Effects of Long-Term Vagus Nerve Electrical Stimulation Therapy on Acute Cerebral Infarction and Neurological Function Recovery in Post MCAO Mice
Date
2022-03-29
Journal Title
Journal ISSN
Volume Title
Repository Usage Stats
views
downloads
Citation Stats
Abstract
<jats:p>Background. Vagus nerve stimulation therapy is proven to produce neuroprotective effects against central nervous system diseases and reduce neurological injury, having a positive effect on the recovery of neurological functions in mouse model of stroke. Objective. This study was aimed at exploring a wider time window for VNS treatment, investigating the long-term behavioral improvement of long-term VNS in mice after pMCAO, and exploring the antiapoptotic properties of VNS and its role in autophagy, all of which may be a permanent deficiency potential mechanism of neuroprotection in hemorrhagic stroke. Methods. Permanent focal cerebral ischemia and implantation of vagus nerve stimulator were performed through intracavitary occlusion of the right middle cerebral artery (MCA). The vagus nerve stimulation group received five times vagus nerve stimulation from 6 h after surgery for 5 days. Adhesive removal test and NSS neurological score were used to evaluate the neurological deficit of mice. TTC staining of mouse brain tissue was performed one week after surgery in order to assess the area of cerebral infarction. Additionally, frozen sections were stained with Fluoro-Jade B to observe the apoptotic cells in the ischemic penumbra of brain tissue. Finally, Western blot was used to detect the changes in the levels of apoptosis-related proteins such as cleaved-caspase3 and Bcl-2 and autophagy-related proteins such as mTOR, Beclin-1, and LC3-II in brain tissue. Results. VNS can effectively reduce the behavioral score of pMCAO mice; TTC results showed that VNS could effectively reduce the infarct area after pMCAO (<jats:inline-formula> P < 0.05 </jats:inline-formula>). After VNS intervention of the pMCAO group compared with the pMCAO+VNI group, the FJB-positive cells in the VNS group were significantly decreased (<jats:inline-formula> P < 0.05 </jats:inline-formula>); Western Blot analysis showed that the expression of cleaved-caspase3 in the brain tissue of mice increased after pMCAO (<jats:inline-formula> P < 0.05 </jats:inline-formula>), and the expression of Bcl-2 decreased (<jats:inline-formula> P < 0.05 </jats:inline-formula>). This change could be effectively reversed after VNS intervention (<jats:inline-formula> P < 0.05 </jats:inline-formula>). Conclusion. VNS could effectively improve the behavioral performance of mice after permanent stroke in addition to significantly reducing the infarct size of the brain tissue. The mechanism may be related to the effective reduction of cell apoptosis and excessive autophagy after pMCAO by VNS.</jats:p>
Type
Department
Description
Provenance
Subjects
Citation
Permalink
Published Version (Please cite this version)
Publication Info
Du, Li, Zhenxing Yang, Huaxin Sheng, Min Liu and Qian Sun (2022). Effects of Long-Term Vagus Nerve Electrical Stimulation Therapy on Acute Cerebral Infarction and Neurological Function Recovery in Post MCAO Mice. Oxidative Medicine and Cellular Longevity, 2022. pp. 1–9. 10.1155/2022/8131391 Retrieved from https://hdl.handle.net/10161/24855.
This is constructed from limited available data and may be imprecise. To cite this article, please review & use the official citation provided by the journal.
Collections
Scholars@Duke
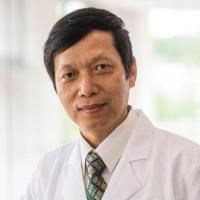
Huaxin Sheng
We have successfully developed various rodent models of brain and spinal cord injuries in our lab, such as focal cerebral ischemia, global cerebral ischemia, head trauma, subarachnoid hemorrhage, intracerebral hemorrhage, spinal cord ischemia and compression injury. We also established cardiac arrest and hemorrhagic shock models for studying multiple organ dysfunction. Our current studies focus on two projects. One is to examine the efficacy of catalytic antioxidant in treating cerebral ischemia and the other is to examine the efficacy of post-conditioning on outcome of subarachnoid hemorrhage induced cognitive dysfunction.
Unless otherwise indicated, scholarly articles published by Duke faculty members are made available here with a CC-BY-NC (Creative Commons Attribution Non-Commercial) license, as enabled by the Duke Open Access Policy. If you wish to use the materials in ways not already permitted under CC-BY-NC, please consult the copyright owner. Other materials are made available here through the author’s grant of a non-exclusive license to make their work openly accessible.
